Hereditary breast and ovarian cancer: What’s your risk?

Of the approximately 300,000 new cases of breast cancer in the U.S. each year, 12 to 14% of those cases can be linked to known gene mutations inherited from one’s mother or father. About 20,000 of U.S. women will receive a new diagnosis of ovarian cancer, and the hereditary link to that cancer is much greater: approximately 1 out of 4 (24%).
“Knowing more about your own hereditary risk can go a long way in helping you take steps that can prevent these cancers,” said oncologist Sydney Brehany, MD, of Rocky Mountain Cancer Centers, who co-presented a free online health lecture with certified genetic counselor Breanna Roscow, MS, CGC, of Myriad Genetics, on “Identifying Your Risk for Hereditary Breast and Ovarian Cancer.”
________________________
Watch "Identifying Your Risk for Hereditary Breast and Ovarian Cancer”
________________________
Identifying hereditary cancer
Genes are found in every cell in the body. They tell each cell when to grow, work, divide and die. When a gene changes or mutates (called a gene mutation), the instructions it gives to the cell can stop it from working properly.
While all cancers are caused by a changes in genes or damage to genes that occur over time, not all cancer is hereditary. “The difference between hereditary cancers and those caused by genetic changes that happen mostly by chance is that hereditary cancers are passed through generations,” said Dr. Brehany.
Breanna further explained that there are particular “red flags” or clues that indicate if there may be a genetic cause for cancer. These clues help doctors and clinicians know if it’s necessary to proceed with genetic testing. The “red flags” in a family history include:
- Cancer at an early age—typically cancer is diagnosed at an older age, seeing it develop in a family member at a younger age is an indication that the cancer may be hereditary.
- Diagnosis of rare cancers (for example ovarian cancer or male breast cancer)—might be a clue that a cancer is hereditary.
- Multiple cancers—could be the person themself, a person in the family or an unusual number of family members being diagnosed with cancer.
Identifying these risks allows us to manage these risks and potentially prevent the cancer from developing.
Breanna noted, “Someone with a hereditary gene mutation associated with breast cancer may have up to an 87% risk of developing breast cancer in their lifetime; for ovarian cancer this risk may be up to 63%.
How is genetic testing done?
“Genetic testing uses either a blood or saliva sample to collect DNA. The sample is sent to a lab by your health care provider, where particular variants or mutations are identified,” explained Breanna.
She offered a cautionary note about “direct to consumer tests” that are available online, indicating, “They’re not as sensitive as the test your health care provider will order, and they may miss a mutation that may be important for you to have identified. Additionally, the FDA has issued a warning about these genetic tests.”
Test results can be either negative, positive or a variant of uncertain significance (VUS). “A VUS,” explained Breanna, “means that we aren’t sure about whether or not a variant identified has been linked to cancer. Additional research may be necessary to classify the variant.”
“A question often asked is,” said Breanna, ‘Will this testing affect my insurance or employment?’ The answer is ‘no.’ There is a federal law called GINA that prohibits discrimination based on genetic testing.” She also noted that genetic testing is often commonly covered by insurance.
Surveillance for hereditary breast cancer
BRCA1 (BReast CAncer gene 1) and BRCA2 (BReast CAncer gene 2) are genes that produce proteins that help repair damaged DNA. Those who inherit harmful mutations in one of these genes have increased risks of several cancers—most notably breast and ovarian cancer.
“Once we know that an individual has been diagnosed with a mutation in one of the hereditary BRCA genes, we begin advocating for breast awareness. This means being sure our patients are familiar with their breasts and knowing if and when any changes occur,” said Dr. Brehany.
General Medical Management for Individuals with a BRCA1 or BRCA2 mutation
According to the National Comprehensive Care Network (NCCN) guidelines, these are the medical management recommendations for patients with a BRCA1 or BRCA2 mutation:
- Female breast cancer surveillance:
- Breast awareness begins at age 18
- Clinical breast exams every 6 to 12 months starting at age 25
- Annual breast MRI starting at age 25
- Annual mammogram (in addition to MRI) starting at age 30
- Male breast cancer surveillance:
- Breast self-exam training and education starting at age 35
- Annual clinical breast exam starting at age 35
- Consider annual mammogram starting at age 50 for BRCA carriers
Note: Management will be customized based on the age of cancer onset in the family.
Treatment options for cancer risk reduction after an initial breast cancer diagnosis
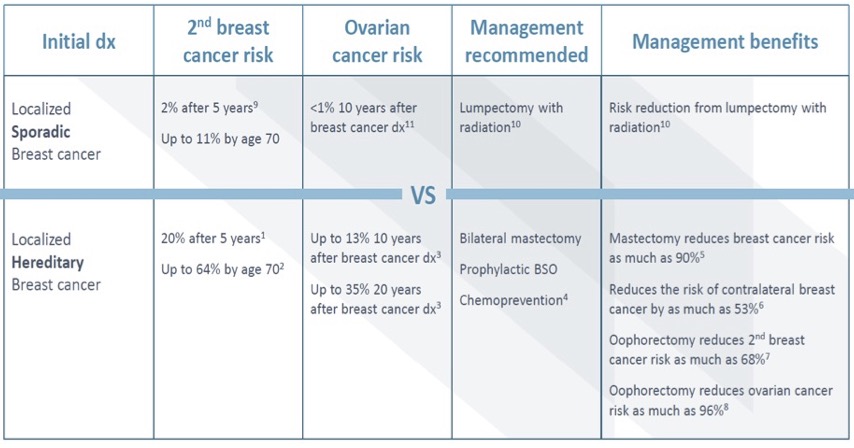
The chart above shows the risk, following an initial breast cancer diagnosis, of a second breast cancer occurring, ovarian cancer occurring, management recommendations and management benefits for localized sporadic (those without an inherited mutation) breast cancer versus localized hereditary breast cancer.
Dr. Brehany explained treating patients with hereditary cancer syndromes and a diagnosis of breast cancer is more involved than patients without a hereditary cancer syndrome. These patients may be offered more aggressive surgery and different medications to try and reduce the risk of future cancers.
Medication options for breast cancer risk reduction
Dr. Brehany presented the various medications that can be used to reduce breast cancer risk in people who have not been diagnosed with cancer. There are two categories:
1. Selective Estrogen Receptor Modulators (SERMs)
- Tamoxifen
- Raloxifene
2. Aromatase Inhibitors—used in post-menopausal women
- Exemestane
- Anastrozole
“After five years of using these medications, we expect the breast cancer risk to be reduced by up to 50%,” said Dr. Brehany.
Ovarian cancer
“Ovarian cancer can be difficult to detect early unless the disease has spread. Symptoms are not always noticeable; they can be vague and may persist for a while before they’re noticed and can be difficult to distinguish from normal menstrual symptoms. However, if the cancer is diagnosed early, 93% of patients may live longer than 5 years after the diagnosis,” said Dr. Brehany.
Symptoms include:
- Bloating
- Trouble eating or feeling full quickly
- Fatigue
- Abnormal bleeding or discharge from the vagina
- Pelvic pain or pressure
- Abdominal or back pain
- A change in bathroom habits, such as more frequent or urgent need to urinate
Surveillance for ovarian cancer
Dr. Brehany shared, “The screening tests available for ovarian cancer are not ideal. They may provide false results and may not help to improve the long-term outcome. As a result, screening is not routinely recommended.”
Oral contraceptive pills can sometimes be used to reduce the risk of ovarian cancer by up to 50%. Your doctor can help you decide if that is an appropriate strategy.
If hereditary cancer is a concern
Hereditary cancer is the least common reason that people are diagnosed with cancer, however, if you believe you may be at risk, schedule an appointment at Rocky Mountain Cancer Centers by calling 303-385-2000. Bring to the appointment your family history and any testing results that have been shared with you by other family members who have been diagnosed with cancer.
Click here to view/download a PDF of slides shown during the lecture.