Prostate Cancer Screening: 'Make an Informed Choice,' Says Dr. Fronczak

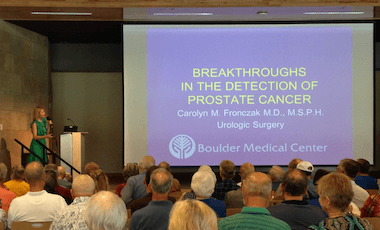 “Despite its high incidence, if found early, prostate cancer is one of the most survivable forms of cancer. Early detection is key,” urologist Carolyn Fronczak, MD, told a crowd of nearly 100 people during a free health lecture held on July 26 in Boulder.
“Despite its high incidence, if found early, prostate cancer is one of the most survivable forms of cancer. Early detection is key,” urologist Carolyn Fronczak, MD, told a crowd of nearly 100 people during a free health lecture held on July 26 in Boulder.
Informed decision-making
While screening for prostate cancer can find it early, leading medical organizations disagree about who should — and who shouldn't — get screened.
“Sometimes screening misses the cancer, and sometimes it finds cancer that turns out to be an unaggressive cancer,” Dr. Fronczak explained.
That’s why the American Cancer Society recommends informed decision-making when it comes to having a test to check for prostate cancer.
“Men shouldn’t rush into routine prostate cancer screening, but instead have full, thoughtful conversations with their doctors about the uncertainties, risks and potential benefits of screening. Together, you and your doctor can decide whether screening is right for you,” said Dr. Fronczak.
The discussion about prostate cancer screening should begin at:
- Age 50 for men who are at average risk of prostate cancer.
- Age 45 for men at high risk of developing prostate cancer. This includes African Americans and men who have a first-degree relative (father, brother or son) diagnosed with prostate cancer at an early age (younger than age 65).
- Age 40 for men at even higher risk (those with more than one first-degree relative who had prostate cancer at an early age).
Screening Tests
There are two main screening tests for prostate cancer:
- Prostate-specific antigen (PSA) test. This is a blood test to check the level of prostate-specific antigen in your blood. Most healthy men have PSA levels under 4 nanograms per milliliter of blood. However, PSA has a limited sensitivity for prostate cancer detection. A lower PSA level doesn’t guarantee a man is free of prostate cancer, and a higher level doesn’t mean he has prostate cancer.
- Digital rectal exam (DRE). During a DRE, a physician inserts a gloved, lubricated finger into your rectum to examine your prostate, which is next to the rectum. Your doctor will assess the size of the prostate and feel for any bumps or hard areas on the prostate that may need to be tested for cancer.
Dr. Fronczak said, “A DRE should be done in all men with an abnormal PSA.”
Diagnosing Prostate Cancer
According to Dr. Fronczak, a standard initial evaluation combines PSA testing with DRE to help identify prostate cancer.
If the results of the PSA and DRE suggest that you may have prostate cancer, your doctor might recommend a prostate biopsy, which involves using a needle, guided by a rectal ultrasound, to remove samples of prostate tissue. The tissue samples are then sent to a lab, where a specialist will determine whether it contains cancer cells.
“However, standard biopsy has risks of pain, infection and may miss the lesion,” Dr. Fronczak warned. “Because of this, the new school of thought is to first recommend prostate MRI to help identify whether a suspicious lesion may be a cancer or noncancerous tissue.”
Multiparametric MRI
At BCH, urologists and radiologists collaborate in using Multiparametric (mp) MRI technology for prostate cancer diagnosis.
mpMRI helps not only determine who needs a prostate biopsy but also assists urologists in performing targeted and precise biopsies. “We also use it to follow men with elevated PSAs but who have had a negative prior prostate biopsy — just to make sure we didn’t miss a lesion, since traditional prostate biopsies are essentially random biopsies,” Dr. Fronczak said.
While still new technology, MRI-TRUS fusion technology for prostate cancer biopsy and diagnosis is being used more and more. This technology blends (fuses) images from an MRI scan and live TRUS.
“This is the latest testing improvement for detecting prostate cancer. It can show hard-to-find lesions and increases finding high-risk tumors by 18 percent,” stated Dr. Fronczak.
Novel Biomarkers
Urologists are also using biomarkers — molecules secreted by a tumor — in blood and in prostate tissue to better diagnose prostate cancer. This technology helps to distinguish between insignificant and significant prostate cancer, as well as identify particularly aggressive cancer.
“Biomarkers give us a probability of finding cancer before proceeding with a biopsy and decrease unnecessary biopsies. Still, biomarkers will not detect all cancers,” said Dr. Fronczak. “At this time, no one biomarker can be recommended over another because of the lack of head-to-head clinical trials.”
Treatment
If prostate cancer is found, treatment options depend on several factors, including how fast the cancer is growing, how much it has spread and the patient’s overall health, as well as the potential benefits or side effects of the treatment.
Treatment for prostate cancer can include active surveillance, radiation therapy, chemotherapy, hormone therapy and surgery to remove the prostate, including robot-assisted prostatectomy surgery.
To schedule an appointment with Carolyn Fronczak, MD, call 303-440-3093.
Click here to view PowerPoint slides from Dr. Fronczak’s lecture on “Detecting and Treating Prostate Cancer.”
Want to receive notification of special events and lectures? Sign up to receive email notifications.